By Claire Bacon, ACN, CNC
If you’re like most midlife women, your body might be changing in unusual ways. Your moods may fluctuate, and your cycle is undependable. It doesn’t take much to make you anxious. Situations you used to look forward to and handle with ease can leave you feeling overwhelmed and irritable. You may think, “am I in menopause?” Maybe, but probably not yet. Changes in hormones on the way to menopause could be a 10-year process (oh joy!). But luckily, there are lots of things you can do to feel better along the way.
Menopausal Changes in Estrogen
Hormone imbalances cause many women to overreact to things that never used to faze them. Imbalanced (high) estrogen could make your breasts feel sore and may lead to lumps, fibroids and cysts. Whereas low levels of estrogen can deflate breast tissue, and could also worsen incontinence, hot flashes, and vaginal dryness.
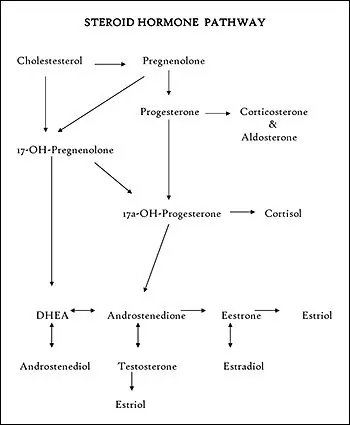
The main estrogens—estrone (E1), estradiol (E2), and estriol (E3)—fluctuate throughout our life stages.
- The body creates Estrone (E1) by enzyme activity on our existing E2 and E3.
- Estradiol E2 is the strongest estrogen that delivers signals to most estrogen receptors, and the one that’s highest in our reproductive years.
- Estriol E3 is a gentler estrogen. It sends anti-cancer signals and keeps our skin soft and supple throughout menopause.
A landmark study in 1989 conducted by Swedish researchers looked at breast cancer risks in over 23,000 users of hormone replacement therapy. The study appeared in the New England Journal of Medicine. The investigators found that Estriol (E3) did not increase breast cancer risks. Rather, it was long-term use of unopposed Estradiol (E2) (unbalanced by progesterone) that increased the risk of breast cancer. This risk goes even higher with use of synthetic progestins. In a follow-up study in 2003, the researchers concluded that indeed, continued use of HRT with synthetic progestins rendered the highest risks for breast carcinoma.
Three Types of Estrogen
Estrone (E1) is a significant estrogenic hormone contributor in BOTH pre and postmenopausal women and in men, too. It is heart and brain protective. Our fat cells make Estrone. Menopausal women need to watch out for out-of-balance Estrone levels, as they are suspect for promoting hormone-driven cancers.
Estradiol (E2) delivers the most powerful estrogenic signals compared to E1 and E3. It protects and directs reproduction, heart, bone, vocal and digestive health and more. E2 protects the lungs from aging and disease, it protects the vocal chords from that “old lady” scratchy voice. Also, it protects the hippocampus, the short term memory center deep inside your brain.
Estriol (E3) is the weakest compared to the other two forms of estrogen. Estriol levels rise in pregnant women and provide anti-inflammatory and gut healing effects. This is one reason why many women with inflammatory conditions (like MS and inflammatory bowel diseases) go into remission during pregnancy. Estriol (E3) is so anti-inflammatory, some doctors use it by intramuscular injection in MS patients to reduce brain plaques and symptoms. Furthermore, E3 has pain protective effects against the development of arthritis. Estriol is even beneficial for interstitial cystitis and inflammatory bowel diseases, because it reduces inflammation and pain. Dating back to the 1960s, the evidence has strongly suggested that estriol may protect against breast cancer. Women who develop breast cancer have too little estriol relative to the more potent estrogens (estradiol and estrone) circulating in their bodies and that women with breast cancer generally had the lowest levels of estriol.
Functions of Estrogen
Estrogens protect. Many diseases (such as Parkinson’s, Alzheimer’s, Tourette’s, attention deficit hyperactivity disorder, osteoporosis, and heart disease) are more apt to occur or get worse in women after menopause (when estrogens go down). Some diseases get better during pregnancy when unique estrogens (like estriol) go up. Partum-related depression can occur when these high pregnancy hormone levels plummet after giving birth or make the thyroid dysfunctional for a period of time. This demonstrates an overall protective and greatly influential effect of changing levels and ratios of estrogens to how we feel, our vulnerability to diseases and our health or lack of it.

Menopausal Changes in Progesterone
Progesterone is the sister hormone to estrogen, working in tandem with it to regulate and protect the health of the reproductive system throughout our fertile years. Among its many vital functions, progesterone governs the second half of the menstrual cycle and is essential to maintaining a pregnancy to term. It also plays a part in the regulation of blood sugar levels, has inherent calming properties, and protects breast, brain and bone health. When it comes to breast cancer prevention, progesterone’s most important role in the body is to balance estrogen.
Estrogen and progesterone primarily come from the ovaries. Unlike estrogen, ovulation is the necessary trigger to produce progesterone. The ruptured follicle that releases an egg upon ovulation then pumps out progesterone for the rest of the cycle. So if and when we don’t ovulate, our bodies do not produce enough progesterone to keep estrogen levels in check—and that sets us up for estrogen dominance. In a nutshell: progesterone deficiency = estrogen dominance = heightened risk for breast cancer. Lack of ovulation, whether it occurs naturally as the result of aging ovaries, or unnaturally, from extremes of stress, exercise, diet, and/or use of synthetic hormones in HRT or birth control pills, will cause estrogen to drop from 40 to 60 percent (enough to stop the menstrual cycle), but progesterone levels plummet much lower, to nearly zero in some women.
Balancing effects from Progesterone:
Only just a few benefits from sufficient progesterone levels: (wink, wink)
- Maintains a nourishing uterine lining,
- Protects against fibrocystic breasts,
- Helps use fat for energy,
- Natural anti-depressant and diuretic,
- Facilitates thyroid hormone action,
- Normalizes blood clotting,
- Restores sex drive (along with testosterone),
- Normalizes blood sugar levels,
- Normalizes zinc and copper levels,
- Restores tissue oxygen levels,
- Helps prevent endometrial and breast cancer,
- Stimulates osteoblast bone building,
- Restores strength of blood vessels.
Remember that without progesterone, estrogen can become toxic to the body. Unopposed estrogen can become a potent promoter of breast cancer.

Menopausal Changes in Adrenal Function
Testosterone
Although testosterone is present in much smaller amounts in women than in men, it has a wide range of essential functions for a woman’s health. These include maintaining libido and sexual function, as well as the normal growth and renewal of muscles, bone and other tissues. Levels of testosterone and its precursor, DHEA, decrease in women at menopause, and are often particularly low in women who have a “surgical menopause” (removal of the ovaries). This is when symptoms of “androgen deficiency” can start to become apparent. Along with the most noticeable effect of lowering libido, low testosterone and DHEA can also result in decreased bone and muscle mass, depression, and vaginal dryness.
Cortisol
Cortisol—the adrenal hormone that maintains the immune system and manages our stress-coping response 24 hours a day—should be highest in the morning when we need to “get up and get going,” and decrease steadily to its lowest point at night, when we need to sleep. When cortisol levels are out of balance, we tend to feel “tired and wired” all the time and/or may suffer from asthma and allergies, chemical and noise sensitivities, anxiety, and eating disorders. We may find ourselves crashing in the afternoon, craving sugar and caffeine to cope, and catching every cold and flu bug that comes along. The bottom line is adrenal exhaustion: when the body can no longer keep up with the demand for constant cortisol.

Menopausal Changes in Thyroid Hormone
Thyroid hormone regulates metabolic rate, so low levels tend to cause unwanted weight gain, depression, low energy and cold intolerance. High thyroid levels (hyperthyroidism) cause “hyper” energy levels, a feeling of being too warm all the time, and persistent weight loss. But it is hypothyroidism (low thyroid) that is most common in women during the peri-menopausal and postmenopausal years. When estrogen is not counterbalanced with progesterone, excess estrogen can block thyroid hormone from being delivered to the cells of the body. This is because high estrogen levels increase proteins (e.g. thyroid binding globulins) that can bind up thyroid hormones and inactivate them, thus making them unavailable to the body. Persistent estrogen dominance (i.e. lack of progesterone) creates a vicious cycle of lowered thyroid function that sets women up for sluggish metabolism, foggy brain, and maybe even an increased risk of cancer.

Monitoring Bioidentical Hormones
If you are currently using bioidentical hormones, it is essential to monitor periodically with a saliva or urine test. Your medical doctor likely only uses serum (blood) testing. Blood does not reveal the “free” circulating hormone that is directly felt at the cellular level. In order to see the “free” levels, we recommend a DUTCH test. It stands for Dried Urine Test of Comprehensive Hormones. It’s the best way to check your levels and your downstream metabolic pathways.
It is way too easy to overdose yourself when using exogenous hormones every day. When that happens, your receptors can become saturated and shrink back – to effectively absorb less hormone. Therefore, the same amount of hormone stops working as well. Your natural instinct may be to add more, but this will only perpetuate the vicious cycle.
In this case, your best bet may be to do a 21-day Purification Cleanse. Doing so can clear out excess hormones, then start back at a lower level, to feel better results. We often recommend that bioidenticals are only used about 2 or 3 days a week. You want to find the absolute tiniest dose that helps you feel your best.
Vitamin D3 as a Balancer for Hormones
Vitamin D is in fact, not a vitamin at all but a hormone. It synthesizes through the action of sunlight upon precursors (i.e. the substances from which hormones are derived) within the skin. Undiagnosed vitamin D deficiency is now considered to be epidemic among the elderly, who stay indoors much of the time. High sunlight exposure, because it promotes the formation of vitamin D, is associated with a lower risk of breast cancer.
Vitamin D’s anti-cancer benefit is because it stops the uncontrolled growth of cells. It promotes their natural differentiation and death (apoptosis), before they can mutate and become cancerous. Vitamin D is breast-protective because it inhibits the blood supply that feeds tumors in malignant breast tissue.

Changes with Hot Flashes and Night Sweats
For some women, hot flashes and night sweats are infrequent and manageable. But for others, these symptoms are intense. Hot flashes and night sweats can easily interfere with quality of life. The cause may be too much estrogen and too little progesterone. Or, it could be other hormones that come from the adrenals, ovaries, thyroid, pancreas or GI tract.
Common culprits: Sugar #1!!! Alcohol – especially wine #2!! After that – starchy foods, smoking, caffeine, fatigue, stress, and lack of muscle-building exercise.

Is there a Quick Fix?
Oh, don’t we wish!! Unfortunately, hormones are too complex to play a guessing game. You really need to test if you want to know what’s going on. But if you would like to get started on a few proactive supplements, we have no problem with that…
You’ll need something for your adrenals:
- Adrenal Desiccated – a fast-acting glandular extract, or
- Ashwagandha Complex – so wonderfully restorative to the HPA axis!
- Adrenal Complex – a blend of Rehmannia and Licorice herbs. Available in-office only.
And your thyroid:
- Prolamine Iodine Plus – a hefty 3 mg of iodine per tablet, or
- Thytrophin PMG – especially important if you have autoimmunity.
Some calming B vitamins to help your stress:
- Cataplex B2 – considered a nervous system tranquilizer, or
- Min-Chex – a favorite for all ages! Especially when feeling emotional!
And our favorite hormonal support herbs for menopausal years:
- Wild Yam Complex – contains Wild Yam, Shatavari, St. John’s Wort, Sage, Korean Ginseng, and Black Cohosh. Great for progesterone support.
- Bone Complex – contains Epimedium, Kudzu, Red Clover and Black Cohosh. Very useful for osteoporosis and natural estrogen support.
- Tongkat Ali – reduces Sex Hormone Binding Globulin (SHBG) to naturally increase testosterone.
- FemCo – contains White Peony, Shatavari, and Schisandra. We often say this one is “for the woman with 100 husbands” because it helps so much with stress and vitality.
- Valerian Complex – contains cooling herbs like Valerian, Passionflower, and Jujube seed that can help you sleep so much better!

Need Some Help?
Reach out to us anytime if you need some direction. We’re happy to get you set up with the right kind of testing. It will be the best way to understand how your hormones are changing inside!
Like this Article?
If you like this article, check out several more just like it…


