By Claire Bacon, ACN, CNC
Hypothyroidism is an extremely widespread condition, affecting as many as 15% of adult women. Thyroid issues may be caused by autoimmunity, maybe triggered by Epstein Barr virus. Or, it could simply be a downregulation of hormone production due to lack of iodine and/or excess gluten or fluoride (common toxins). Regardless of the cause, hypothyroidism is 8 to 9 times more likely to develop in women than men. As we get older, especially beyond 80 years old, the risk of being hypothyroid in men catches up to that of women.
Physiologically, thyroid hormones affect multiple body systems:
- the ability to manage blood pressure and regular heart rhythm
- mental alertness and memory
- cardiac output, cardiac oxygen consumption, and exercise performance
- peripheral or systemic vascular resistance (SVR) aka swelling
- overall weight control
- cellular detoxification and liver function
- body temperature
- kidney function (filtration and fluid balance).
Thyroid hormones T4 (inactive) and T3 (active) have the ability to increase contractility or strength of the heart muscle, increase heart rate, and metabolism. They are also involved various processes of detoxification and fluid balance. The thyroid is in control of many body processes, and certainly in order to be healthy, you want your thyroid hormones to be perfectly optimized.
However, the thyroid is very sensitive, and many factors can alter how it maintains this fine equilibrium. Nutritional deficiencies may leave your thyroid at a disadvantage to producing enough or converting enough hormone. Chemical exposure to the halogen elements fluoride, chlorine, and bromide might be blocking the thyroid receptors. And conditions such as adrenal exhaustion, liver congestion, and anemia may impair the thyroid’s ability to do its work properly.
Thyroid Physiology
Let’s take a look at how thyroid hormones work in the body, and how you may feel if things aren’t working right…
Basic Physiology of Thyroid Hormones
The thyroid exerts its action on almost every cell and organ in the body through production of Thyroxine (T4). As long as the diet supplies plenty of nutritional cofactors and toxicity doesn’t get in the way, the thyroid “should” produce the T4 you need.
Producing T4
Top nutritional needs (and therapeutic foods) for the thyroid include:
- iodine (from seafood and seaweed)
- selenium (from Brazil nuts)
- vitamin E (from wheat germ and almonds)
- iron (from red meat and cooked spinach)
- l-tyrosine (an amino acid found in meat)
- zinc (oysters, red meat, crab, lobster, and pumpkin seeds)
- B vitamins (eggs, legumes, citrus fruits, and avocado)
- Vitamin D (from sun exposure, cod liver oil, and salmon).
I say the thyroid “should” produce T4 because it is made in response to Thyroid Stimulating Hormone (TSH), which comes from the pituitary gland. So, when you ask your doctor to check your thyroid and he only looks at TSH, he’s really checking activity from your pituitary gland!
Your doctor’s assumption is that the hypothalamus and pituitary glands in the brain are always working properly. The hypothalamus perceives how much thyroid hormone is in the system, and it communicates through its own TRH to the pituitary what it thinks about the need for more. In most cases, this is a pretty good system. However, common factors such as trauma or stress can alter the function of either gland, and impact the TSH independent of whether you actually have normal thyroid hormones in the system.

Converting to T3
The thyroid gland primarily secretes T4, which is converted to active T3 hormone in the liver, kidney, and skeletal muscle.13,14 If you have dysfunction in any of these organs, you’ll likely have impaired conversion to T3 (Triiodothyronine). This is the most common reason so many people can’t lose weight and have no energy, yet their TSH and T4 might look fine in bloodwork. It’s because the problem is in the conversion process!
Nutritional factors (and foods) that help with proper conversion from T4 to T3, and cellular absorption include:
- Selenium (from Brazil nuts)
- Zinc (from oysters, red meat, crab, lobster, and pumpkin seeds)
- Vitamin A (carrots, butter, yellow bell peppers, squash)
- Vitamin D (sun exposure, cod liver oil, and salmon).

What Happens Next…
From there, your T3 hormone will convert into T2 (3,5-diiodo-L-thyronine) and that’s the form that will actually run your metabolism. There is no test for T2 just yet, so doctors typically assume you’ll have adequate T2 if you have enough T3. Beyond that, there is another thyroid hormone called T1, but only academics are studying it. It hasn’t reached clinical use yet.
No one really talks about T2, but there are a few supplements that contain T2 and claim to help with fat loss and metabolism. I think the jury is still out on whether T2 supplements are helpful or could be harmful. In my personal experience, the one I tried was helpful during a time when I was hurt and unable to exercise normally. I did not feel any adverse side effects. However, the scientific literature has not yet come to the same conclusion.
Common Symptoms You Might Not Connect with Thyroid
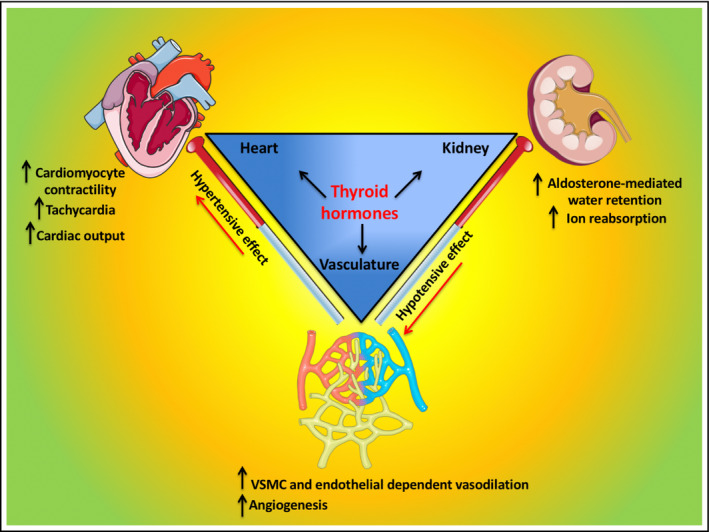
Thyroid hormone also affects the vasculature – as in small capillaries throughout the muscle tissue. Lack of T3 can change how the body balances sodium, potassium, and calcium. If your electrolytes are off, you may notice changes in energy, blood pressure, or brain fog.
In one study, researchers found that the higher the TSH level one had, the higher the magnesium and phosphorus levels were in the blood, and the lower the values of serum calcium, sodium, and potassium levels were. Electrolyte imbalances like this may result in muscle cramps, depression, constipation, or irregular heartbeat.

Cardiac symptoms of hypothyroid include:
- Bradycardia (very slow heart rate)
- High diastolic blood pressure
- Longer QT interval, which may lead to ventricular irritability
- Low tolerance to physical exercise (sucking wind in your favorite sport).
T3 directly upregulates mitochondrial biogenesis and ATP production. These are big words that just mean ENERGY PRODUCTION. Do you want to feel better, with more “get up and go?” Then T3 hormone may play a part in your solution.
Thyroid hormone, when sensed in the kidneys, activates the renin-angiotensin-aldosterone system. This increases renal sodium absorption and erythropoietin synthesis, which increases the number of red blood cells and your ability to carry oxygen in the blood. In untreated hypothyroidism with a lack of T3, cardiac output may decrease by 30% to 50% due to this lack of red blood cells and oxygen.
Wow! If you’re wanting to improve your 5k time, you better get your thyroid levels under control!
Thyroid Hormones’ Action on the Heart
The heart relies mainly on serum T3 to provide its driving force. The cardiac myocyte is a specialized muscle cell within the heart that controls muscle contraction and proper electrical activity. Only T3 is transported into the myocyte. If you are low in T3, you will feel when you’re running that you’re working SO HARD but going nowhere. You may see a very high heart rate even though you’re barely above a walk. Without T3, the cardiac cells become very inefficient and simply can’t work. It literally feels like you’re hitting a wall. Don’t ask me how I know!
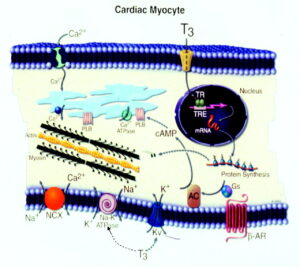
T3 does a few other things within the heart. It regulates intracellular calcium cycling, enhances contractile function, and allows diastolic relaxation (when the chambers are refilling with blood). ATP production (for energy) is also under T3 regulation.
Hypothyroid Arteries and Nitric Oxide
Thyroid hormones T3 and T4 are able to decrease systemic vascular resistance (SVR), which means that generalized puffiness you feel in your lower legs can go away. Part of this process involves enhanced nitric oxide production due to the activation of AKT signaling pathways, which are protective of the endothelial lining in the arteries and the heart.
If you’ve heard me talk about the endothelial lining before, it was probably in the context of high blood pressure. Yes, there may be a definite connection between being hypothyroid and high blood pressure!
In chronic hypothyroidism, endothelial function is reduced. You could think of this as “arterial stiffening” or systemic vascular resistance (SVR). In other words, persistent swelling and puffiness. Basically, if your nitric oxide availability is reduced, you may find: your blood pressure creeping up, brain fog getting worse, poor circulation worsening, and… get this… even lack of orgasms.
If you haven’t caught my drift so far, being chronically hypothyroid is no way to go through life!

More About Thyroid Hormone and Blood Pressure
T3 directly increases renin and aldosterone secretion in the liver, and increases blood volume. But without it, hypothyroidism causes a rise in diastolic blood pressure (the bottom number). Because cardiac output is low, the pulse pressure is narrowed. The increase in diastolic pressure with low T3 is a sodium-sensitive form of hypertension.
But don’t worry too much. When thyroid hormone therapy is properly dosed, most people experience a significant lessening in their symptoms. That’s why it’s so important to properly test your levels! More on that later.
Hypothyroid Effects on Cholesterol
Hypothyroid people tend to have elevated Total Cholesterol levels, often with high low-density lipoproteins (LDLs) and Apolipoprotein B. The reason is because low thyroid hormone causes reduced LDL clearance in the liver due to reduced receptor activity.
In addition, when you’re hypothyroid, other things in the liver may slow down. The process that changes cholesterol into bile involves the enzyme “7α-hydroxylase”. T3 regulates this enzyme, and a deficiency may cause decreased function. The result may be a buildup of cholesterol and inadequate bile. This can easily cause constipation.
If left untreated, the situation of high cholesterol along with diastolic hypertension may be predisposing factors to atherosclerosis. Something you definitely don’t want! We recommend that everyone over 40 get a Coronary Calcium Score test. You don’t know if you don’t test!
Thyroid Effects on Kidney Function
Hypothyroidism negatively affects the kidneys. Because of the “arterial stiffness” or vaso-constriction, the sensitive, small capillaries in the kidney tighten. This process decreases the eGFR (estimated Glomular Filtration Rate). As a result, less sodium and chloride can be absorbed into the kidneys, and this could contribute to acute kidney injury.
Worst case scenario, being in a hypothyroid state for many years could cause permanent damage to the kidney. However, if you catch it early enough, thyroid hormone therapy can restore eGFR – even with stage 2–4 chronic kidney disease.
Sadly, hypothyroidism is associated with higher mortality in Dialysis patients. Studies show that low levels of T3 predict poor outcomes in such patients. But, good news! Properly restored levels of T3 and T4 can decrease the risk of cardiovascular complications and can benefit kidney health.

How to Evaluate Thyroid Hormones
With all this talk about high levels and low levels, you may be wondering, “Am I at risk?” Unfortunately, medical doctors are typically NOT evaluating thyroid levels properly in your yearly physical. IMO, 9 out of 10 are completely uneducated on how to understand the full thyroid picture.
Even if you ask to check your doctor to check your full thyroid panel, usually he will only check TSH. I think we’ve already established that TSH is an incomplete assessment.
Best Thyroid Lab Markers
That’s why, when we order lab work in our office, we try to include all of these markers:
- T4 and Free T4 (make sure you’re producing enough)
- Free T3 (the active hormone you want)
- Reverse T3 (if stressed, conversion could lead to this dead-end hormone)
- TSH (the pituitary signal to the thyroid, to do more or less)
- TPO and Tg antibodies (evidence of autoimmune attack)
Dr. Weston Childs has some good insight here on what constitutes “normal values” and appropriate levels of medication for hypothyroid conditions.

Plus, we like to order a few nutritional markers, like:
- Iron and Ferritin (necessary for T4 production)
- Vitamin D (helps with conversion)
- Lipids (sign of excess inflammation)
- Vitamins B6 and B12 (involved in energy processes)
- Magnesium, RBC (deficiency impacts immune and thyroid functions)
- Homocysteine and C-Reactive Protein (because they relate to arterial inflammation).
Not all of these things may fit in the budget at first. But we can definitely prioritize your most important things to check first.
Favorite Supplements for Optimizing Thyroid
Wouldn’t it be nice to get all the nutrients we need from our diet? Sorry folks, it’s not going to happen!
Here are our favorite supplements for improving thyroid function:
- Thytrophin PMG – to encourage normal growth and repair of the thyroid gland
- Thyrostim – a multivitamin for the endocrine system, with hypothalamus and pituitary extracts
- Prolamine Iodine – a good dose of iodine to fuel the thyroid and protect against fibrocystic breasts
- Thyroid Complex – an alternate source of iodine from Bladderwrack
- Black Cumin Seed Forte – if there is autoimmunity
- Rehmannia Complex – contains Hemidesmus herb to help with autoimmunity. Available in office.
- Thyrotain – helpful to promote conversion from T4 to T3. Although you may still need to take T3! Available in office.
- GTA Forte – a stronger dose of key thyroid nutrients when TSH is trending high

Plus, don’t forget some adaptogens for adrenal function, as well as some detoxifying support for the liver!
In addition to the above, if you are lacking in T3, you need to get on T3! Hypothyroid symptoms all tend to resolve when you have the proper dosage of T3!
Speak with your doctor about how you’ve been feeling, and present him with complete test results to justify your need. We can help you with this if you’re having trouble getting proper testing.
Bottom Line
Give us a call, and let’s figure out what might be underlying your symptoms. You owe it to yourself to learn how to nourish your thyroid back to health!
Like this article??
Check out a few more related articles…


